Cataracts
Inside your eye, there is a natural lens that is normally clear. Over the years, changes in the eyes lead to the breakdown of the lens’ proteins, causing them to become cloudy. This film is what we refer to as cataracts.
Symptoms of cataracts include:
- Hazy, blurry vision
- Greater sensitivity to glare and light
- Yellowing of colors
- Dim vision
- Double vision that’s in just one eye
- Needing more or brighter light for reading and similar activities
- Difficulty with driving, especially at night
- Seeing rings or halos around lights
While cataracts are a common condition associated with aging, there are other risk factors that could increase your chances of developing them or having them appear earlier in your life. Risk factors include:
- Excessive sunlight exposure
- Past eye surgery
- Excessive alcohol use
- High blood pressure
- Diabetes
- Extended use of corticosteroid medications
- Previous eye inflammation and/or injury
- Obesity
- Genetics
____________________________________________________________________________
Glaucoma
Glaucoma is an eye disease that causes damage to your optic nerve. It typically results from a build-up of fluid in the front part of the eye. The pressure caused by this extra fluid damages the optic nerve, leading to blindness. If left untreated, glaucoma can result in permanent blindness in just a few years.
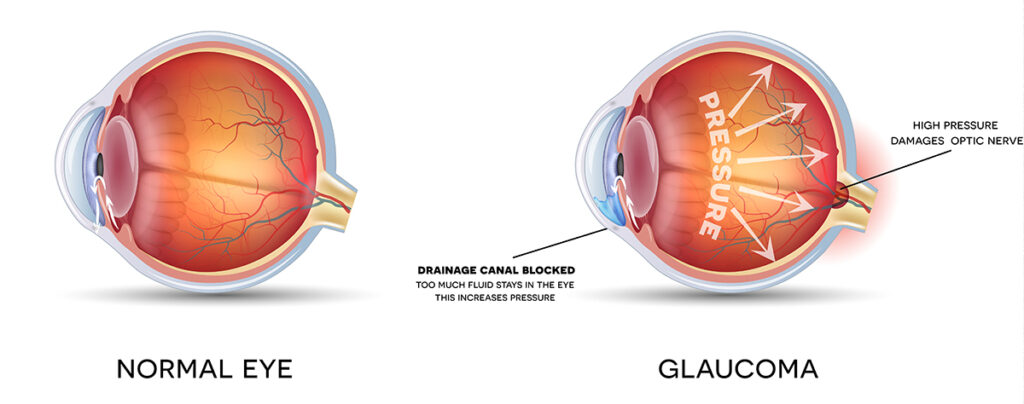
There are two primary types of glaucoma:
- Open-angle glaucoma (a.k.a. wide-angle glaucoma) is the most common. With this type of glaucoma, your eye’s drainage system looks normal but the fluid doesn’t leave the eye as it’s designed to do.
- Angle-closure glaucoma is more common in Asia than in Western countries. It is also sometimes called chronic angle-closure glaucoma or narrow-angle glaucoma. This type of glaucoma is marked by the drain space between your cornea and iris narrowing. This can cause your intraocular pressure to suddenly buildup. Farsightedness and cataracts are also associated with this type of glaucoma.
Glaucoma doesn’t usually display any symptoms in the early stages, which is why early detection during yearly eye exams is essential. The following are some common symptoms of glaucoma:
- Halos surrounding lights
- Redness in your eyes
- Vomiting and/or nausea
- Eye pain
- Loss of peripheral vision
- Narrowed, or tunnel, vision
Anyone can develop glaucoma, but in most cases, it affects adults age 40 and older. Other risk factors include:
- Diabetes
- Trauma to the eye
- Taking certain medications such as prednisone
- Family history of glaucoma
____________________________________________________________________________
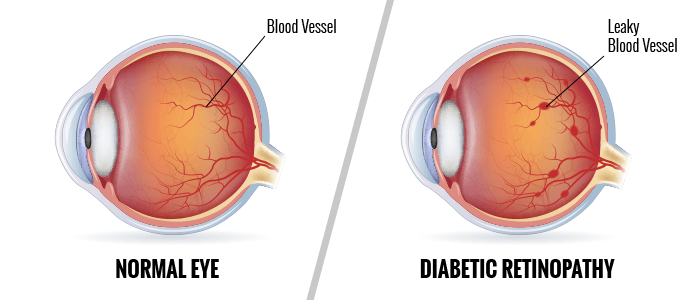
Diabetic Retinopathy
Diabetic retinopathy is a serious complication of diabetes that affects your eyes. It is the number one cause of vision loss in diabetic patients. Diabetic retinopathy is caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). This causes bleeding, swelling, and abnormal blood vessel growth. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye condition.
Symptoms of severe diabetic retinopathy include:
- Empty or dark areas within your line of vision
- Fluctuating vision
- Dark strings and/or spots (i.e. floaters) in your vision
- Loss of vision
- Reduction in color vision
Management of your diabetes under the care of a medical professional — with a treatment plan that includes regular visits to the eye doctor — is the best way to prevent loss of vision.
If left untreated, complications can include:
- Vitreous hemorrhage: The centers of your eyes are filled with a jelly-like substance that’s clear. Blood vessels formed by diabetic retinopathy could leak into this vitreous jelly and cause floaters or even block your vision completely.
- Retinal detachment: The presence of abnormal blood vessels encourages the growth of scar tissue in the retina. This could pull the retina away from its position at the back of your eye. Common symptoms of a retinal detachment include flashes of light, severe loss of vision and/or spots floating in your vision.
- Glaucoma: If the abnormal blood vessels that mark the presence of diabetic retinopathy grow into your eye’s front area, they could block the normal flow of fluid from your eye. The result could be glaucoma which is an increase in the eye’s pressure. You might experience damage to the optic nerve if it’s left untreated.
- Blindness
____________________________________________________________________________
Age-related Macular Degeneration (AMD)
Age-related macular degeneration — abbreviated as AMD — is a disease of the retina, the light-sensitive portion of your eye. The retina is located at the back of the eye, and the macula is a small area near the very center. Your macula is responsible for your central vision.
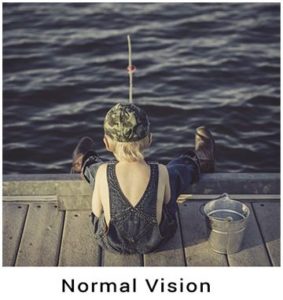
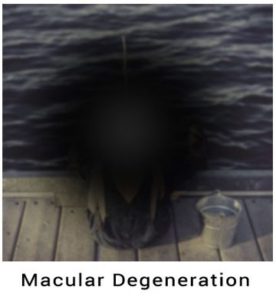 In AMD, the macula loses its ability to detect light, resulting in a partial or total loss of central vision. People with late-stage AMD are unable to see objects straight in front of them, making it difficult to perform many activities, like using a computer, reading, driving, or recognizing faces. AMD typically causes no symptoms until vision begins to fade. Having routine eye exams, especially over age 50, is important for catching AMD as early as possible. There is no cure for AMD. Instead, people who have AMD require treatments that help slow the progression of the disease, which is why early detection is very important.
In AMD, the macula loses its ability to detect light, resulting in a partial or total loss of central vision. People with late-stage AMD are unable to see objects straight in front of them, making it difficult to perform many activities, like using a computer, reading, driving, or recognizing faces. AMD typically causes no symptoms until vision begins to fade. Having routine eye exams, especially over age 50, is important for catching AMD as early as possible. There is no cure for AMD. Instead, people who have AMD require treatments that help slow the progression of the disease, which is why early detection is very important.
Age is the biggest risk factor for AMD, followed by having a family history of AMD. You’re also at greater risk of developing AMD if you are:
- Caucasian (white)
- Female
- Have had prolonged sun exposure
- A smoker or past smoker
- Genetic predisposition
There are two types of AMD: dry and wet. The dry type is much more common, but the wet type is more severe and also develops more quickly. If you have the wet form of AMD, medications or laser therapy may help slow your vision loss. Otherwise, treatment focuses on monitoring the progression of the disease, along with taking nutritional supplements and incorporating the lifestyle changes listed above.
_________________________________________________________________________________________________
Dry Eye Syndrome
Dry eye is a condition that can be chronic or temporary, where people cannot produce enough tears to nourish the eye. Luckily crying is not the only way to cover you eye with tears, every time you blink you produce a film of tears that spreads over the eye, keeping your eye surface smooth and clear of debris. When this protective coating dries up, the eyes may feel “gritty” or burn and can be more sensitive to light. In extreme cases, vision can be blurred. Often daily activities, like working on a computer can cause infrequent blinking which could lead to dry eye.
Symptoms of dry eye include:
- Burning sensation
- Itchy eyes
- Aching sensations
- Heavy eyes
- Fatigued eyes
- Sore eyes
- Dryness sensation
- Red eyes
- Photophobia (light sensitivity)
- Blurred vision
- Foreign body sensation — the feeling that grit or something is “in” your eye.
- Watery eyes: dryness on the eye may sometimes over-stimulate tears as a protective measure. This reflex through does not stay long enough to nourish the eye.
____________________________________________________________________________
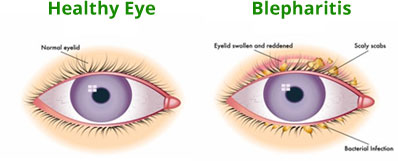
Blepharitis
Blepharitis is a general term for an inflammation of the eyelid and eyelashes. It is among the most common and stubborn eye conditions usually resulting from poor eyelid hygiene, a low-grade bacterial infection (usually staphylococcal), an allergic reaction and/or abnormalities in oil gland function. Like some other skin conditions, blepharitis can be controlled but not cured. The main goals in treating it are to reduce the amount of bacteria along the lid margin and open plugged glands.